Stifle Arthroscopic TPLO in 6-year-old castrated Labrador Retriever – by Nathan Squire, VMD, MS, DACVS-SA
HISTORY
One-month history of left hindlimb lameness (grade IV/V) with acute onset. The patient had a history of intermittent forelimb lameness that would resolve after 1-2 days of rest. Lameness was minimally responsive to carprofen. The previous response to the Librela administration for forelimb lameness was less than desirable.
PHYSICAL EXAM
The left stifle had moderate intracapsular effusion and moderate medial buttress. There was moderate instability (both cranial tibial thrust and cranial tibial drawer), as well as an intermittent meniscal click. The patient also demonstrated pain with the McMurray test, involving stifle hyperflexion and internal rotation. Discomfort was noted with stifle hyperextension. There was mild bilateral thickening of the hocks and mild crepitus, but no pain was noted with manipulation. Both forelimbs were noted to be orthopedically normal. Incidentally, there was a 2.5 x 1 x 1 cm soft, freely movable, subcutaneous mass on the medial aspect of the left antebrachium.
DIAGNOSTICS
A fine needle aspirate and cytology of the left forelimb mass were performed and were consistent with a lipoma. A routine complete blood count and chemistry panel were performed and were unremarkable. Radiographs were performed of the left stifle (Figure 1), which revealed moderate to significant intracapsular soft tissue opacity (consistent with joint effusion), very mild osteophytosis at the proximal aspect of the femoral trochlear ridges and the insertion site of the cranial cruciate ligament (CCL) on the tibial plateau, as well as moderate cranial tibial subluxation. No other concerning changes were noted.

Figure 1
SURGICAL PLAN
Left stifle arthroscopy and tibial plateau leveling osteotomy (TPLO)
ARTHROSCOPIC FINDINGS AND SURGERY
A complete tear of the CCL was noted, and an arthroscopic shaver was used to debride the torn fibers (Figure 2). To evaluate the medial meniscus, valgus stress was placed on the limb, and the arthroscope was directed medially. A bucket handle tear of the meniscus was identified (Figure 3). The bucket handle tear is released via transection with an arthroscopic punch, and the abaxial portion of the tear is debrided (Figure 4). The axial portion of the tear (the meniscotibial ligament) is subsequently debrided to remove the entirety of the tear (Figure 5). Following meniscectomy, the caudal aspect of the medial compartment of the joint is probed thoroughly to interrogate for additional bucket handle tears (Figure 6).
Figure 2

Figure 3
The medial femoral condyle is at the top of the image, the cranial horn of the medial meniscus is at the bottom left of the image. An arthroscopic probe can be seen underneath the bucket handle tear of the caudal pole of the meniscus, retracting the torn portion of meniscus cranially. Note the significant number of frayed fibers that are typically indicative of chronicity.
Figure 4
Figure 5
Figure 6
The lateral aspect of the joint was then explored, and mild axial fraying of the lateral meniscus was noted (Figure 7). This is a common finding in patients with chronic CCL tears. No treatment was performed.

Figure 7
A routine TPLO was then performed and secured with a 3.5 mm broad, locking TPLO plate (VOI, Versiv). The tibial plateau angle (TPA) had been measured as 25 degrees on the preoperative radiographs. Postoperative radiographs revealed a TPA of 5 degrees consistent with the planned correction, good compression across the osteotomy site, and appropriate implant placement. Also note that the cranial tibial subluxation has been resolved (Figure 8).
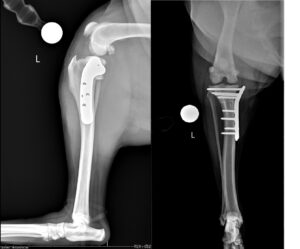
Figure 8
OUTCOME
The patient recovered routinely from anesthesia and surgery and was discharged the following day. The owners elected to pursue formal physical therapy with the GCVS Sports Medicine and Rehabilitation, as is routinely recommended following most orthopedic surgeries. The patient was evaluated at 8 weeks postoperatively, at which point the left hindlimb lameness had resolved and muscle atrophy had markedly improved. Palpation of the left stifle revealed a full and comfortable range of motion with mild crepitus noted. No discomfort was noted on direct palpation of the surgical implants, and cranial tibial thrust was absent. Consistent with the TPLO mechanism of function, the cranial tibial drawer remained moderate. No meniscal click was noted, and the patella tracked normally. Radiographs were performed and revealed complete osseous union of the previous osteotomy with mild bony callus formation at the caudal aspect. The implants remained static, and there was no evidence of implant-associated infection. Mild intracapsular soft tissue opacity (consistent with effusion) was noted. There was equivocal thickening of the patellar ligament near the insertion site on the tibia (Figure 9).
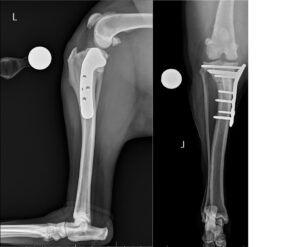
Figure 9
DISCUSSION
Medial meniscal tears have been documented in as many as 44% of canine patients with CCL tears (Plesman et al 2013). When left untreated, latent meniscal tears cause ongoing pain, lameness, muscle atrophy, and more rapidly progressive osteoarthritis. Arthroscopy is considered the gold standard for intraarticular evaluation in the canine stifle and other joints and is superior for diagnosing meniscal pathology (with up to 15% of meniscal tears potentially being missed with routine arthrotomy) (Pozzi et al, 2008). Arthroscopy also allows for evaluation of other important intraarticular structures, such as the articular cartilage of the patella and femoral trochlear groove, common locations for osteochondritis dissecans (OCD) lesions, such as the articular surface of the lateral femoral condyle, caudal cruciate ligament injury, and the lateral meniscus, to name a few. Caudal cruciate ligament evaluation is especially important given that incompetence of this ligament is a contraindication to the TPLO procedure.
Arthroscopy is a specialized procedure with a steep learning curve. It necessitates highly specialized equipment, but it is a crucial part of the complete evaluation of the canine stifle joint, particularly when treating CCL tears, the most common cause of lameness in the canine hindlimb. This case demonstrates the diagnosis and arthroscopic treatment of a bucket handle tear of the medial meniscus, leading to a successful recovery and return to excellent function and quality of life for the patient involved.
